Join the live stream for the #IndabaGrandChallenge kickoff meeting on YouTube on Tuesday 30 June 3pm Accra,Dakar (UTC) | 4pm Abuja,Kinshasa,Yaounde | 5pm Johannesburg,Lilongwe | 6pm Nairobi, Kigali.
https://www.youtube.com/c/deeplearningindaba/live
Leishmaniasis is a neglected disease. As a disease of poverty, it has historically received limited funding for discovery, development and delivery of new tools. Current treatment is costly, lengthy, painful and sometimes toxic. Like a handful of similar diseases, it is the scourge of whole regions affected by them, because we still miss cheap, safe and effective cures for them.
At the same time, new drug candidates are being developed and old ones are being tested every day. Today, millions of drug activity assays are available at the press of a button. In this Indaba Grand Challenge, we dare to ask you to help identify amongst the already known, tested and (often) approved drugs, potential cures for different forms of leishmaniasis.
Leishmaniasis
Humanity has been remarkably successful in curing most of communicable diseases, be it of bacterial or viral origin. However, there remains a whole group of diseases that largely evade successful treatment – the ones transmitted by parasites. Large number of them is caused by a group of small, single-celled animals named kinetoplastids. They cause such diseases as African sleeping sickness (caused by Trypanosoma brucei), Chagas disease (Trypanosoma cruzii) and Leishmaniasis (different Leishmania species).

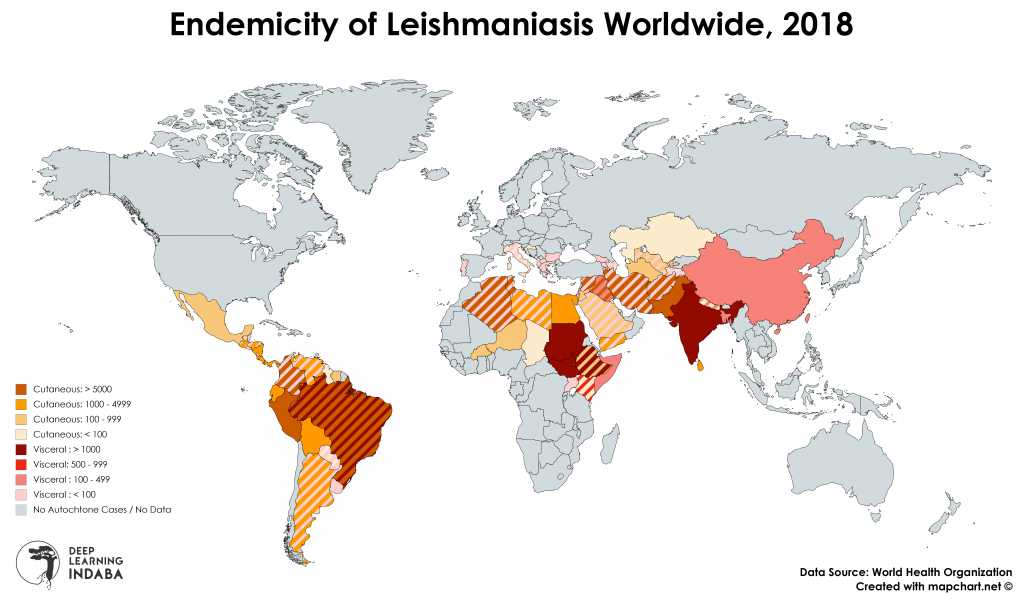
Leishmaniases (as it is a whole group of diseases), are spread by bites of sandflies and readily communicated between animals (such as dogs). Out of 30 species that attack animals, 21 affect humans. There are more than 350 million people in nearly 90 countries, that live in areas where leishmaniasis is common. Around 90% of its most dangerous variant – visceral leishmaniasis – is recorded in Bangladesh, Nepal, Sudan and Brazil, but disease is prevalent also in Mexico, South and Central America, Asia (excluding the South-East Asia), Middle East, southern Europe and Africa (in particular North and East Africa) .
Every year approximately 12 million people are afflicted with the disease, with over 2 million new cases each year, most of which is a cutaneous (skin) leishmaniasis (nearly 1.5 million), but nearly 25% comprises the most lethal, visceral variant. Parasite suppresses the host’s immune system to avoid eradication, which often leads to frequently lethal secondary respiratory infections. Yearly, approximately 50 thousand people die worldwide because of Leishmania caused diseases.
Visceral leishmaniasis causes swelling, malaise, wasting, damages spleen and liver, as well as leads to characteristic graying of skin (hence the name black fever). The fever caused by the disease lasts for more than two weeks and does not abate with antimalarial drugs. The cutaneous type makes for wide-spread sores that can take over a year to heal, and lead to necrosis (dying of tissue). It leads to scars on the face, neck, arms and legs. The third, mucocutaneous type causes both skin and mucosal ulcers, leading to the damage of soft tissues and cartilage, predominantly of nose and mouth area. All types tend to co-occur with AIDS (approximately 1 in 60 AIDS patients in south of France suffers from leishmaniasis).

The treatment for visceral leishmaniasis is problematic and relies mostly on antibiotics, which have a variable success rate. The most commonly used non-antibiotic drugs, containing pentavalent antimony (such as sodium stibogluconate or meglumine antimonate) are toxic to the heart, kidneys, pancreas and bone marrow of the patient, leading to headaches, abdominal issues, vomiting and low levels of blood platelets. They also require a month-long treatment through injections, as medication does not work well if taken by mouth. There is no safe treatment for cutaneous leishmaniasis, that would work dependably, with fluconazole (an antifungal medication) and pentamidine (an antimicrobial used for other kinetoplastid diseases) being the most promising support medications. Miltefosine, the first promising oral treatment for visceral leishmaniasis, tends to be effective for cutaneous form, but has limited use, as it is known to cause birth defects.
In the recent years a massive drug discovery campaign has led to discovery of a new drug (codenamed GNF6702) and its analog (a new, improved version, named NITD689), which affect parasites ability to degrade unnecessary and damaged proteins. While these drugs seem to work against a wide range of pathogens (including these causing African sleeping sickness, Chagas disease and visceral leishmaniasis), they are not effective against the other leishmaniases. Additionally, there is an emerging mutation among the parasites, that already now renders the drug ineffective. Therefore, even though it is currently successful in the clinical trials, it will most likely not lead to the eradication of the disease.
There is a dire need for a new, safe therapy for kinetoplastis, one that can be administered earlier, with lesser likelihood of bothersome side effects, one that could eradicate these diseases once and for all. Finding this therapy is the goal of this Indaba Grand Challenge, and literally lives are at stake. The approach to identify potential cure candidates is drug repurposing.
What is Drug Repurposing?

Drug repurposing is the act of researching if an existing drug can be used for new therapeutic purposes. It’s something that has been done for centuries. A large amount of medications on the market right now are used for multiple purposes: for instance, aspirin is a pain reliever and also a blood thinner, ibuprofen is also used for pain relief, and for reducing inflammations.
The high cost of research and development involved in finding new drugs means that most of these will be targeted to “First World” countries to generate returns.
For “neglected diseases” or “tropical diseases”, drug repurposing is used as a sort of universal strategy: it lowers the costs of research and production and the time needed for clinic trials, which is why you’ll find that many of these diseases use medication that was originally used for other illnesses.
The Challenge
Drug discovery methods and pipelines are well described and modular. Each can be decomposed into smaller pieces, which can be rearranged and modified. All of these pipelines rely heavily on knowledge representation, pattern detection and building of statistical models.
The goal of this Indaba Grand Challenge is to, through the use of standard techniques and publicly available data on drugs, drug targets and kinetoplastids (parasites causing amongst other leishmaniasis), identify either:
- Compounds among known, approved drugs which can target known drug targets in Leishmania (especially one of the 15 species known to cause the cutaneous type of disease) in addition to their official use.
- Compounds among known, approved drugs with sufficiently similar targets in the goal organisms to the targets in kinetoplastids.
Importantly, the verification of a drug-target interaction is possible and routinely done in silico. However, not all drug-target combinations can be verified, due to sheer combinatorial expansion and limited computational resources. In addition, the identification of similarities and analogies between known experimental data is far from trivial and, despite the existence of numerous approaches, cannot be solved by one statistical technique alone.
By launching this Grand Challenge, and true to the core values of Deep Learning Indaba, we aim to build a collaborative effort, joining experts and enthusiasts in machine learning and software engineering, with doctors, epidemiologists, medicinal chemists and policy experts, to create a synergistic effect at scale. Our vision, if it becomes true, is one where interesting discoveries of the community are taken up by the experts, and conclusions of the experts are fed back to the community to iteratively improve on its findings and make breakthroughs possible. No single person can do it perfectly, but through a joint effort, together we can.
Challenge Specs
Goal: Propose a new treatment, comprising an Leishmania protein (either from a defined species, or a protein present in the proteome of one or more of the Leishmania species) and a small molecule (or set of small molecules). Submission can be specified as:
- Small molecule (SMILES/SMARTS string or SDF file) and a protein name
- PDB file with a structure of a target and a bound small molecule
Available resources: We have put together a list of available resources and additional material here.
Who can apply?
We invite you to join this initiative and help put an end to Leishmaniasis. We need your involvement, especially if, you are:
- Data science or Machine Learning expert or enthusiast: we have the data, tools, benchmarks and everything you need to know to attack this problem. Our community needs your data wrangling skills. If you feel up for a challenge, apply here!
- Bioinformatics and Cheminformatics people: in addition to the resources, data and standardized protocols, we have a community, which can help you go the final mile from a great protocol to a great candidate. We need your expertise in translating life into bytes. If you can help, please apply here!
- Kinetoplastid researchers, practitioners and clinicians. We need you dearly. We will be generating loads of hypotheses and we need you to help make sense of them. We need you to answer questions, we cannot answer ourselves. In return, we will give you a fresh, new insight to the problem you care about. Please apply here to help us cure this scourge!
- Universities, institutes and research organizations. We know it is difficult to find either meaningful project work for students, or dedicated people to do the work with you. If you feel your students would enjoy working with cutting edge methodology, in a collaborative discovery environment, that includes everyone, please do not wait any longer with contacting us. If your research can contribute to this project, we would be deeply grateful, if you could join us. Even if you want to bounce some ideas, we want to hear from you. Apply here and join the truly collaborative effort to democratise drug discovery!
- NTD-oriented organizations and policy makers: We need you more than ever – this project will result in viable drug candidates. We will need a lot of good will to get them to the people in need. We also need access to those, for whom African trichomoniasis is their life work, experts and field workers. We need their expertise. You have the ear of those who matter for us the most. We work to help advance your cause. Together, we can make a difference. If you believe that together we can make a difference, please do apply here!
- Companies in Machine Learning/AI, Bioinformatics or other: If you’re interested in making a valuable contribution to the success of this Grand Challenge, there are multiple ways you can help. What’s straightforward but important is to provide cash or cloud computing credits, as this is a quantitatively intensive project that will make extensive use of GPUs and cloud compute power. You can also contribute in kind with access to your platform or technical expertise like some of the companies already participating in this initiative (see list below, or even better join the list).
If you are excited about this project, but do not belong to any of the categories listed, if you have comments, questions or just want to say hi – we want to hear from you! There is no voice too quiet or contribution too small to make a difference. We need community ambassadors, spokespeople, word-of-mouth champions. We need everyone. We need you, let’s make it happen!
You can find more information in the FAQs page.
Grand Challenge Partners
[sponsors]
Recent Comments